 The core business of hospitals is patient care, often baked with teaching and research.
The core business of hospitals is patient care, often baked with teaching and research.
But wait — there’s more, asserts the Lown Institute in their approach to ranking America’s Best Hospitals in 2020.
The Institute’s methodology for assessing what’s “best” addresses ten pillars. Several of these are the “stick-to-the-knitting” components of the Webster Dictionary definition of hospital work: patient outcomes, clinical outcomes, avoiding overuse, patient safety, and a recent focus, patient satisfaction.
Community benefit has been part of a hospital’s life, especially in the not-for-profit world where hospitals must demonstrate goodwill generated for and provided in the neighborhoods in which they operate.
 Then there’s more, Lown Institute notes:
Then there’s more, Lown Institute notes:
- Civic leadership
- Inclusivity
- Pay equity, and
- Value of care.
Patient outcomes earn the greatest weight in the index, and that’s why larger hospitals tend to do better in this ranking algorithm. That’s because larger inpatient settings achieve lower mortality in surgery (the more you do, the better outcomes you have) and most medical conditions.
But that’s a tendency, not necessarily universal: if you look at the top 10 list of Best Hospitals, you’ll find institutions of varying sizes, missions, and geography. Beyond patient outcomes, smaller hospitals tended to score higher on civic leadership and value of care in this analysis.
The top 10 hospitals live in California, Georgia, Massachusetts, Ohio, Oregon, Pennsylvania, and Texas…north, south, east, and west.

The Institute was surprised by the similarity of nonprofit and for-profit hospitals for civic leadership.
“One would expect a bigger difference between these two types of hospitals when it comes to civic leadership, given that most nonprofit hospitals have a stated mission to invest in community health and are expected to do so by Internal Revenue Service regulations,” Lown Institute notes.
In fact, hospitals whether non- or for-profit scored similarly for community benefit and inclusivity. The only significant difference was for pay equity, where nonprofit hospitals demonstrated fairer pay scales.
Still, the level of community benefit demonstrated by nonprofit institutions was lacking for many, an issue that has received media attention in many local markets.
What is also clear is that safety net hospitals, those who care for people with lower-incomes, score lower for outcomes. This was and is not a surprise: these institutions have fewer resources, Lown Institute calls out, and also care for patients with multiple morbidities who also have fewer resources at-hand in real life to deal with social determinants of health.
The report notes:
“These patients are often discharged from the hospital into situations where they are less able to get the continuing care they need. A patient who is discharged to an apartment on the fifth floor of a walk up with no grocery store nearby might not do as well as a patient who can hire an aide to help them recover at home.”
The Lown Institute study was covered in detail here in The Washington Monthly.
 Health Populi’s Hot Points: The Lown Institute’s expansion of a hospital’s punch-list to include civic leadership, inclusivity, pay equity, and value of care strongly resonate in this moment. The U.S. is arm- and heart-wrestling with the convergence of the coronavirus pandemic, economic recession, and civil unrest.
Health Populi’s Hot Points: The Lown Institute’s expansion of a hospital’s punch-list to include civic leadership, inclusivity, pay equity, and value of care strongly resonate in this moment. The U.S. is arm- and heart-wrestling with the convergence of the coronavirus pandemic, economic recession, and civil unrest.
The community benefit component is particularly impactful at this time in America. Check out this useful explanation of community benefit, from CACHE, the Center to Advance Community Health and Equity.
The IRS originally recognized a U.S. hospital can be designated not-profit as a charitable organization providing care to patients unable to pay for it. The IRS expanded guidelines for nonprofit status allowing hospitals to provide “community benefits” in lieu of charitable care. The Affordable Care Act added requirements for nonprofit hospitals’ status, notably conducting Community Health Needs Assessments.
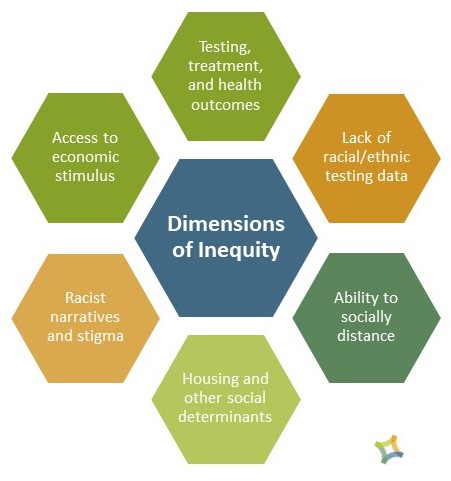
Hospitals have the opportunity to leverage community benefit programs that address health disparities: social determinants and inequities, such as those shown in the diagram developed by the Health Resources in Action organization.
The COVID-19 pandemic has uncovered equity as a root cause of being exposed to, and dying from, the coronavirus.
