A study of gay and bisexual male participants in the first large implementation study of HIV pre-exposure prophylaxis (PrEP) in Australia has found that although rates of bacterial sexually transmitted infections (STIs) were high, they did not increase in the two years after starting PrEP. In contrast, they increased significantly in the year before men started PrEP.
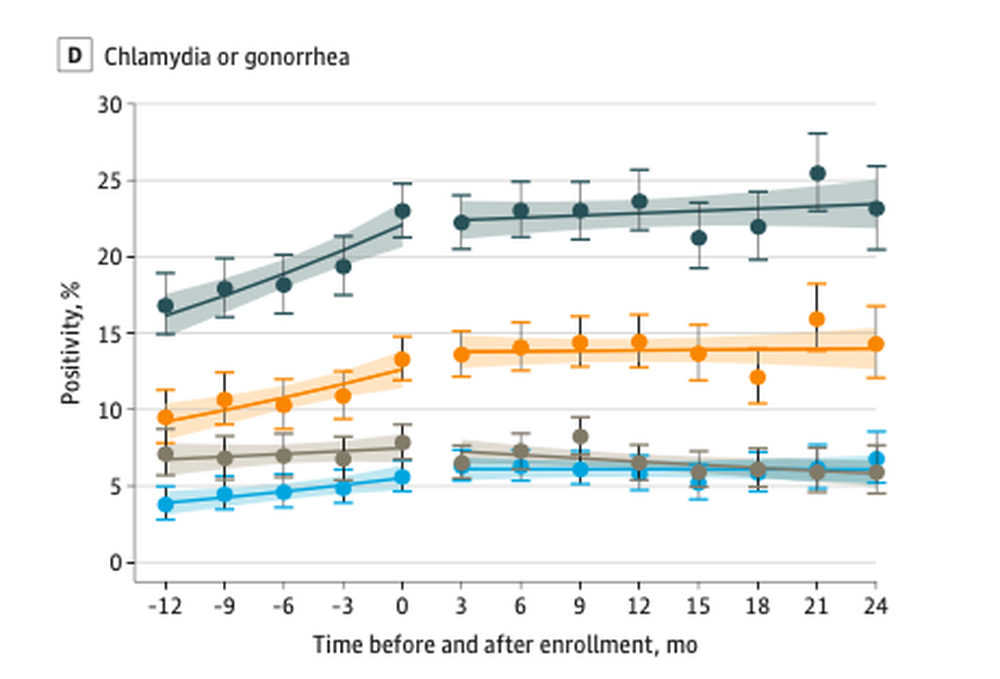
The diagnosis rate per three-monthly period did not change after starting PrEP. In contrast, during the year before starting PrEP, the quarterly diagnosis rate for gonorrhoea and chlamydia increased steadily, from 17% (i.e. one in six study participants) in the first quarter to 23% in the quarter immediately before starting PrEP. This 23% rate was essentially maintained over the following two years on PrEP.
In the year before PrEP 50% of participants were diagnosed at least once with chlamydia, gonorrhoea or syphilis, and 16% were diagnosed twice or more. In the two years after starting PrEP the annual diagnosis rate was 52% and 20% had two or more diagnoses.
This study does show that the men who took PrEP during the two years of EPIC-NSW were at very high risk of STIs. But it does not indicate that starting PrEP, or behavioural changes that might accompany this such as dropping condoms or being more likely to have receptive anal sex, caused STI rates to be higher. On the contrary, it suggests that the behavioural changes that led to increases in STIs preceded the adoption of PrEP.
Background
Whether PrEP directly causes gay men to take greater sexual risks and catch more STIs has been a hotly debated question, and different studies and meta-analyses of studies have come to different conclusions. The evidence is summarised in PrEP in Europe’s research briefing.
The largest meta-analysis, which looked at 17 studies covering 4388 participants, found that in the six months starting PrEP, diagnoses of the three STIs did increase, by 24% overall, and by 39% for rectal infections. However, an Australian study found that the STI increases were concentrated among a minority of the highest-risk men and were partly explained by higher rates of STI testing while on PrEP.
Meta-analyses are able to review large sets of data, but their reliability may be affected if the findings of the studies they cover are very heterogeneous or they use different methods. So it is useful to have a quite large study that follows the same group of people throughout.
The EPIC-NSW study
The Expanded PrEP Implementation in Communities in New South Wales (EPIC-NSW) study was one of the first to show that putting a large number of gay and bisexual men on PrEP did lead to reductions in HIV infections, not only in study participants but in the wider population. The reduction in HIV infections was 97.6% in study participants (there were only two infections, one in someone who never started PrEP) but more remarkably there was a 25% reduction in HIV infections in New South Wales generally and a 32% reduction in recent infections.
The present study looked at 2404 out of the 9709 EPIC-NSW participants who had had at least two tests for gonorrhoea and/or chlamydia in the year before they enrolled in EPIC-NSW, and at least one in the two years after enrolment. A smaller number (1228 or 51% of this study’s participants) had also been tested for syphilis using the same criteria. STI diagnoses prior to enrolment were available from a large national database of sexual health and primary care clinics in a sentinel programme called ACCESS.
EPIC-NSW enrolled participants between March 2016 and April 2018: the span of this study stretches from the beginning of the previous year (2015) to the end of 2018. The small number of EPIC-NSW participants who were not men who have sex with men were excluded, as was anyone who had accessed PrEP, even informally, before joining the study.
The average age of the 2404 men was 35.6. Half of them had been born in Australia, 16% in other high-income countries, and 15% in Asia.
Results
As already mentioned, in the year before EPIC-NSW enrolment, diagnoses of one or both chlamydia or gonorrhoea increased, from 17% at baseline to 23% during the quarter prior to enrolment. Chlamydia diagnoses increased from 8% to 13%, and gonorrhoea from 10% to 14% (higher than the rate after starting PrEP, though not significantly so). The quarterly rate of increase of diagnoses of gonorrhoea and chlamydia during that year was 8%, and this was statistically significant.
In the two years after starting PrEP, the diagnosis rates stayed more or less steady, at a rate of 22-23% per quarter for diagnosis of chlamydia or gonorrhoea (13-14% for chlamydia and 12% for gonorrhoea).
Gonorrhoea and chlamydia were categorised by site of infection. Rectal infections were responsible for most of the increase in infections in the year prior to PrEP, though urethral chlamydia increased too. Pharyngeal (throat) gonorrhoea was the most common site of infection prior to PrEP but actually decreased slightly after PrEP, and became equal in frequency to rectal gonorrhoea; urethral gonorrhoea was less common. Rectal chlamydia was the most common site of infection throughout, with pharyngeal chlamydia the least common.
Syphilis rates did not increase during the whole study, remaining at 2-3% per quarter throughout.
Comments and conclusions
The authors comment that their findings suggest “that previously described increasing incidence of STIs among men taking PrEP mainly reflects a pre-existing increasing trend in STIs in these men.” It is not the only study to find this: a 2017 study from Seattle in the US found rises in all three bacterial STIs in the year prior to starting PrEP. The year after, syphilis rates declined, and gonorrhoea rates stayed flat. Chlamydia did go up, but this may have been due to more STI testing among PrEP users, which could have detected more asymptomatic cases.
The rates of STI tests in the current study did increase after participants started PrEP, from 3.2 tests a year to 4.45. If anything, for reasons similar to the Seattle study, this would tend to increase the number of infections detected after starting PrEP, not before. However, as the authors point out, they selected only the EPIC-NSW participants who had had at least two STI tests in the year before PrEP. This was only a quarter of all participants (and, for syphilis, only an eighth), and these would tend to be those at highest risk already. So we don’t know if STI rates followed a similar trend in the other three-quarters of predominantly lower-risk men.
The lack of any further increase in STI rates during PrEP may be due to there being no further increases in risk behaviour. However, it could also support the argument, advanced by the World Health Organization among others, that frequent STI testing may improve STI detection rates and therefore treatment – and that PrEP could be a catalyst for this.
This finding may seem to contradict recent studies that show that the less common STIs such as LGV and sexually transmitted hepatitis C, previously concentrated among HIV-positive gay and bisexual men, are now more common among HIV-negative men. This may not reflect a general increase in condomless sex, but a greater willingness to have unprotected sex with men of the opposite HIV status, due to PrEP and awareness of U=U.
