This article was previously published May 9, 2018, and has been updated with new information.
For years, opioid addiction in the U.S. has continued to spiral at all-time highs — so much so that, by 2017, it had already been identified as a significant factor in unemployment among men,1 with opioid overdoses the leading cause of death among Americans under the age of 50.2 By 2021 opioid overdoses and deaths were still rising, even though prescribing of the drugs had decreased by 44.4%.3
According to the Centers for Disease Control and Prevention (CDC), of the more than 63,600 Americans who died from drug overdoses in 2016,4,5 more than 42,000 were related specifically to opioids6 — a 28% jump in opioid deaths from the year before. Just five years later, in 2022, the National Center for Drug Abuse Statistics reports that 96,700 deaths every year are now due to drug overdoses, and 72% of those deaths are directly related to opioids.7
The pandemic contributed to a surge of overdoses in 2020 and 2021, reaching record-level deaths just in the first half of 2021.8 Researchers said pandemic restrictions and the high availability of synthetic opioids contributed to this, adding, “The death toll during the first six months of 2021 was an estimated 53,000 people, higher than any continuous six-month period in 2020 and on pace for a new annual record by the end of the year.”
As if that’s not disturbing enough, research9 in the past has suggested opioid overdose deaths were being undercounted by 20 to 35% due to drug omissions on death certificates.10 They were still being underreported in 2020, according to an associate professor of economics at the University of South Florida College of Public Health.11
Undercounts can happen easily, first, because the U.S. government doesn’t track death rates for every drug;12 and second, in many cases, the specific drug that contributed to the death isn’t listed on the death certificate, and it’s quite likely that many of the general “drug deaths” are actually due to opioids specifically. According to NPR,13 a more accurate count a few years ago probably would have put the opioid-related death toll at nearly 40,000 for 2015 and closer to 50,000 for 2016.
Sacklers’ Marketing Schemes Exposed
The most common drugs involved in prescription opioid overdose deaths in 2017 were methadone, oxycodone (such as OxyContin®) and hydrocodone (such as Vicodin®),14 and as shown after multiple litigation settlements by states and others,15 evidence revealed that opioid makers such as Purdue Pharma, owned by the Sackler family,16 knew exactly what they were doing when they claimed opioids — which are chemically similar to heroin — had an exceptionally low addiction rate when taken by people with pain.
In fact, the massive increase in opioid sales was traced back to an orchestrated marketing plan aimed at misinforming doctors about the drug’s addictive potential. Even though the Sacklers continue to claim their innocence in the overmarketing of these drugs, the scheme came to a legal end in December 2021, when a federal judge overturned a $ 4.5 billion settlement that would have protected them from personal responsibility in multiple lawsuits filed by states.
Remarkably, despite widespread discussion about the dangers of opioids and the high risk of addiction, and despite updated treatment guidelines for back pain that stress nondrug interventions over pain killers, and even though doctors slowed down in prescribing these drugs, drug overdoses are continuing to spiral.
What’s Different in 2022, Compared to 2017?
In 2017, the idea that opioids not only were being overprescribed, but that the opioid makers themselves were manipulating the marketing and prescribing of them was just coming to light. In that timespan, multiple states filed lawsuits against Purdue Pharma, as well as against several drug chains and drug distribution agencies.17
By August 2020, 49 states had sued Purdue Pharma in lawsuits totaling $ 2.5 trillion; the drug company responded by denying responsibility and filing for bankruptcy.18 In 2021, strategy consulting firm McKinsey & Company agreed to pay $ 573 million to 47 states, the District of Columbia and five territories for its part in “turbocharging” opioid sales.19
By March 8, 2022, the Sacklers were agreeing to settle for between $ 5.5 billion and $ 6 billion — but still refused to admit any wrongdoing.20 In response to the wave of awareness and the lawsuits, doctors reined in their prescribing of opioids by 44.4% over the preceding years.21 Yet, the American Medical Association (AMA) noted that the country was still facing “a worsening drug-related overdose and death epidemic.”
“The report shows that overdose and deaths are spiking even as physicians have greatly increased the use of prescription drug monitoring programs …” the AMA says on its website. “To address this continuing epidemic, the AMA is urging policymakers to join physicians to reduce mortality and improve patient outcomes by removing barriers to evidence-based care.”
The problem today, the AMA adds, “is mainly due to illicit fentanyl, fentanyl analogs, methamphetamine and cocaine.” What’s worse is that “80 to 90 percent of people with a substance use disorder receive no treatment,” they said. So, if overprescribing isn’t the real issue, what is? What is driving the high overdoses and deaths?
“The nation’s drug overdose and death epidemic has never just been about prescription opioids,” said AMA president Gerald E. Harmon … “Patients need policymakers, health insurance plans, national pharmacy chains and other stakeholders to change their focus and help us remove barriers to evidence-based care.”
When you add fentanyl to the counts, opioid deaths in 2022 outnumber their closest competitor — cocaine — by 3-to-1, killing more than 136 Americans every day.22 Strategies for addressing this include stopping prior authorization for medications to treat opioid disorders and ensuring access to affordable, evidence-based care, the AMA says. But what caused this in the first place?
Paying Doctors to Prescribe Was Part of the Problem
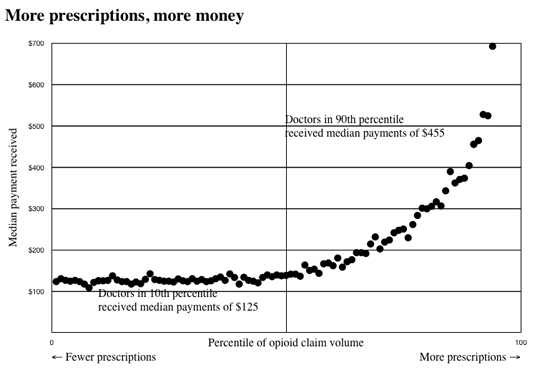
One of the reasons for this appeared early on to be financial. As reported by CNN in 2018, “The more opioids doctors prescribe, the more money they make.”23 According to an analysis by CNN and Harvard researchers, in 2014 and 2015, hundreds of doctors received in excess of $ 25,000 each from opioid manufacturers, and those who prescribed the most opioids received the largest payments.
Dr. Andrew Kolodny, senior scientist at the Institute for Behavioral Health, co-director of the Opioid Policy Research Collaborative and executive director of Physicians for Responsible Opioid Prescribing told CNN, “This is the first time we’ve seen this, and it’s really important. It smells like doctors being bribed to sell narcotics, and that’s very disturbing.”
At least one doctor received more than $ 1 million over those two years. One of his patients, who is struggling with opioid addiction, was shocked when she discovered her doctor had received such large payments from the drug maker. “Once I found out he was being paid, I thought, ‘Was it really in my best interest, or was it in his best interest?'” she told CNN.
Dr. Michael Barnett, assistant professor of health policy and management at Harvard T.H. Chan School of Public Health added, “I don’t know if the money is causing the prescribing or the prescribing led to the money, but in either case, it’s potentially a vicious cycle. It’s cementing the idea for these physicians that prescribing this many opioids is creating value.”
One-Fourth of Doctors Received Payments From Opioid Makers
To assess the link between drug company payments and prescription habits, the team reviewed data from two federal government sources — one that tracks drug company payments to doctors and another that tracks prescriptions made to Medicare patients. Of the 811,000 doctors who wrote prescriptions for Medicare recipients during 2014 and 2015, more than 200,000 prescribed opioids and received payments from the drug makers.
While a majority of them received only minor payments, ranging from $ 100 to $ 1,000, more than 31,400 of them received as much as $ 15,000, and nearly 4,000 of them received more than $ 15,000. As you’d expect with a kickback scheme, those who prescribed the most opioids received the most money. According to CNN:24
“On average, doctors whose opioid prescription volume ranked among the top 5% nationally received twice as much money from the opioid manufacturers, compared with doctors whose prescription volume was in the median. Doctors in the top 1% of opioid prescribers received on average four times as much money as the typical doctor. Doctors in the top 10th of 1%, on average, received nine times more money than the typical doctor.”
And although doctors were prescribing fewer opioids by December 2020, pharma payments to physicians were still delivering a “big return on investment in prescription growth” and “fueling an increase in prescriptions,” according to FiercePharma.25 The payments are mostly consulting and speaker fees but, still, even FiercePharma admitted that in some cases, “the incentives were actually enough to be the main source of a physician’s income.”
Does Your Doctor Have a Financial Incentive?
While it’s legal for drug companies to pay doctors for a variety of services, including speaking and consulting fees — it’s illegal for doctors to prescribe drugs in exchange for kickback payments from the manufacturer. This investigation reveals the line is thin indeed between what’s legal and what’s illegal. Are doctors prescribing opioids or other drugs with the expectation or promise of payment?
At bare minimum, the data provide additional proof that payments influence a doctor’s prescribing habits, even if it’s not wholly intentional. As the 2020 data show, regardless of what the payments are for, when a doctor receives money from a drug company, they are far more likely to prescribe that company’s drugs.
As noted by Dr. Daniel Carlat, a psychiatrist and former director of the Prescription Project at the Pew Charitable Trusts who writes about conflicts of interest in medicine:26
“It’s not proof positive, but it’s another very significant data point in the growing evidence base that marketing payments from drug companies are not good for medicine and not good for patient care. It makes me extremely concerned.”
Did Fentanyl Maker Bribe Doctors to Overprescribe?
In one particularly disturbing case highlighted by CNN, a woman with Crohn’s disease was prescribed Subsys, an “ultrapowerful form of fentanyl” for her abdominal pain by a pain specialist in Greenville, South Carolina. Subsys is up to 100 times more potent than morphine, and while it eliminated her pain, the drug also put her in a “zombie-like state,” making her unable to care for her children. What’s worse, she couldn’t quit.
Skipping a day led to “uncontrollable diarrhea and vomiting,” and when she asked her doctor for another option, “he became belligerent,” saying “it was Subsys or nothing.” As it turns out, this doctor received more than $ 190,000 from the maker of Subsys between 2014 and 2015.
A lawsuit is now pending in which she’s accusing her doctor of “setting out to ‘defraud and deceive’ her for ‘the sole purpose of increasing prescriptions, sales and consumption of Subsys to increase … profit.'”
Incidentally, in October 2017, John Kapoor, the founder of Insys, which makes Subsys, was arrested and charged with bribing doctors to overprescribe the drug. Other Insys executives have also been arrested on racketeering charges.27 In late 2021, Kapoor and some of his fellow executives were ordered to pay $ 48.3 million in restitution for their parts in the opioid crisis.
Were Payments to Doctors Fueling the Opioid Epidemic?
The investigation by Harvard and CNN was not the first to suggest drug company payments were a driving factor in the opioid epidemic. According to a study28 published in August 2017, between August 2013 and December 2015, more than 375,000 non-research opioid-related payments were made to more than 68,000 physicians, totaling more than $ 46 million.
This means 1 in 12 U.S. physicians collected payments from drug companies producing prescription opioids during those 29 months.
Here, fentanyl prescriptions, specifically, were associated with the highest payments, and many of the states struggling with the highest rates of overdose deaths, such as Indiana, Ohio and New Jersey, also had the most opioid-related payments to physicians. In other words, this study showed there’s a direct link between doctors’ payments and patient addiction rates and deaths.
Conflicts of Interest Between Drug Makers and Government
Conflicts of interest that hurt the public also exist between drug companies and the U.S. government. As reported by STAT News,29 the National Institutes of Health (NIH) had originally planned on sharing the cost of a $ 400 million opioid addiction research project with a dozen different drug companies. The goal of the project was to develop new drug addiction medicines and alternative pain killers.
However, after ethics flags were raised by an advisory panel, the agency made a sudden turnabout, announcing it will not accept drug industry contributions after all. Instead, the project would be exclusively funded by taxpayers. STAT News wrote:
“The agency has long pursued such partnerships on disease-specific research … Last year, the NIH announced a separate partnership on cancer immunotherapy, which relies on $ 55 million in funding from drug companies. On the issue of opioids, however, attitudes appear to be dramatically different — largely due to the role many pharma companies are seen to have played in the opioid crisis.
In its recommendations, the NIH advisory committee specifically cited Purdue Pharma and Mallinckrodt, two opioid manufacturers currently being sued for their opioid marketing tactics. ‘There’s so much controversy swirling around pharmaceuticals on the opioid issue,’ said Rep. Tom Cole (R-Okla.), who chairs the House appropriations subcommittee on health …
Cole and others … also cited the ongoing controversy involving Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism, a unit within the NIH. STAT reported this month that Koob had discouraged research on the impact of alcohol marketing after working with beverage industry lobbyists to fund research promoting the benefits of moderate alcohol consumption.”
Could Cannabis Curb the Opioid Epidemic?
In related news in 2018, CNN chief medical correspondent Dr. Sanjay Gupta published an open letter to U.S. then-attorney general Jeff Sessions, in which he urged Sessions to change his stance on cannabis,30 saying “Not only can cannabis work for a variety of conditions such as epilepsy, multiple sclerosis and pain, sometimes, it is the only thing that works … It is time for safe and regulated medical marijuana to be made available nationally.”
Later, in December 2021, Gupta rocked the world by appearing on the Joe Rogan show and explaining why he’d changed his stance to support marijuana.31 He told Rogan that after he did some digging, he found that most of the data were “very biased” and focused on harms rather than benefits of the drug. He had to go outside the country to learn the truth, but once he looked for them, studies showing impressive benefits started popping up.
Gupta cited research from the Rand Corporation, which found a 20% decline in opioid overdose deaths in states that had legalized medical marijuana. “[T]hese data suggest that medicinal marijuana could save up to 10,000 lives every year,” he writes. Not only could cannabis treat the pain itself, lowering or eliminating the need for narcotics, but it can also ease symptoms associated with opioid withdrawal. There’s also no risk of overdose or death using cannabis.
“[P]erhaps most important, the compounds found in cannabis can heal the diseased addict’s brain, helping them break the cycle of addiction,” Gupta notes, adding, “there is no other known substance that can accomplish all this. If we had to … design a medicine to help lead us out of the opioid epidemic, it would likely look very much like cannabis.”
Gupta also provided an example of an individual who received virtually no pain relief from opioids, taking an estimated 40,000 pills over the course of a decade, who suddenly was nearly pain-free after a single dose of cannabis. Indeed, in addition to underestimating opioid’s addictive potential, the drug’s effectiveness against chronic pain has also been vastly exaggerated, further heightening the potential for addiction. As noted in a 2016 paper by the CDC:32
“Most placebo-controlled, randomized trials of opioids have lasted six weeks or less, and we are aware of no study that has compared opioid therapy with other treatments in terms of long-term (more than 1 year) outcomes related to pain, function, or quality of life.
The few randomized trials to evaluate opioid efficacy for longer than six weeks had consistently poor results. In fact, several studies have showed that use of opioids for chronic pain may actually worsen pain and functioning, possibly by potentiating pain perception …”
Treating Your Pain Without Drugs
With all the health risks associated with opioid painkillers, I strongly urge you to exhaust other options before resorting to these drugs. Following is information about nondrug remedies, dietary changes and bodywork interventions that can help you safely manage your pain.
Medical cannabis — As Gupta learned, medical marijuana has a long history as a natural analgesic and is now legal in some form in dozens of states.33 You can learn more about the laws in your state on medicalmarijuana.procon.org.34 |
Kratom — Kratom (Mitragyna speciose) is a plant remedy that has become a popular opioid substitute.35 In August 2016, the DEA issued a notice saying it was planning to ban kratom, listing it as Schedule 1 controlled substance. However, following massive outrage from kratom users who said opioids were their only alternative, the agency reversed its decision.36 Unfortunately, its legal status is still unstable, as the U.S. Food and Drug Administration is on a crusade to eliminate kratom. However, as of 2022 the FDA had yet to take action, choosing instead to allow states and local communities to make their own rules regarding this substance.37 Kratom is safer than an opioid for someone in serious and chronic pain. However, it’s important to recognize that it is a psychoactive substance and should be used with great care. As opposed to marijuana, there’s very little research showing how to use it safely and effectively, and it may have a very different effect from one person to the next. The other issue to address is that there are a number of different strains available with different effects. Also, while it may be useful for weaning people off opioids, kratom is in itself addictive. So, while it appears to be a far safer alternative to opioids, it’s still a powerful and potentially addictive substance. So please, do your own research before trying it. |
Low-Dose Naltrexone (LDN) — Naltrexone is an opiate antagonist, originally developed in the early 1960s for the treatment of opioid addiction. When taken at very low doses (LDN, available only by prescription), it triggers endorphin production, which can boost your immune function and ease pain. |
Curcumin — A primary therapeutic compound identified in the spice turmeric, curcumin has been shown in more than 50 clinical studies to have potent anti-inflammatory activity. Curcumin is hard to absorb, so best results are achieved with preparations designed to improve absorption. It is very safe and you can take two to three every hour if you need to. |
Astaxanthin — One of the most effective oil-soluble antioxidants known, astaxanthin has very potent anti-inflammatory properties. Higher doses are typically required for pain relief, and you may need 8 milligrams or more per day to achieve results. |
Boswellia — Also known as boswellin or “Indian frankincense,” this herb contains powerful anti-inflammatory properties, which have been prized for thousands of years. This is one of my personal favorites, as it worked well for many of my former rheumatoid arthritis patients. |
Bromelain — This protein-digesting enzyme, found in pineapples, is a natural anti-inflammatory. It can be taken in supplement form, but eating fresh pineapple may also be helpful. Keep in mind most of the bromelain is found within the core of the pineapple, so consider eating some of the pulpy core when you consume the fruit. |
Cayenne cream — Also called capsaicin cream, this spice comes from dried hot peppers. It alleviates pain by depleting your body’s supply of substance P, a chemical component of nerve cells that transmit pain signals to your brain. |
Cetyl myristoleate (CMO) — This oil, found in dairy butter and fish, acts as a joint lubricant and anti-inflammatory. I have used a topical preparation of CMO to relieve ganglion cysts and a mild case of carpal tunnel syndrome. |
Evening primrose, black currant and borage oils — These oils contain the fatty acid gamma-linolenic acid, which is useful for treating arthritic pain. |
Ginger — This herb is anti-inflammatory and offers pain relief and stomach-settling properties. Fresh ginger works well steeped in boiling water as a tea, or incorporated into fresh vegetable juice. |
Dietary Changes to Fight Inflammation and Manage Your Pain
Unfortunately, physicians often fall short when attempting to effectively treat chronic pain, resorting to the only treatment they know: prescription drugs. While these drugs may bring some temporary relief, they will do nothing to resolve the underlying causes of your pain. If you suffer from chronic pain, making the following changes to your diet may bring you some relief.
Consume more animal-based omega-3 fats — Similar to the effects of anti-inflammatory pharmaceutical drugs, omega-3 fats from fish and fish oils work to directly or indirectly modulate a number of cellular activities associated with inflammation. While drugs have a powerful ability to inhibit your body’s pain signals, omega-3s cause a gentle shift in cell signaling to bring about a lessened reactivity to pain. Eating healthy seafood like anchovies or sardines, which are low in environmental toxins, or taking a high-quality supplement such as krill oil are your best options for obtaining omega-3s. DHA and EPA, the omega-3 oils contained in krill oil, have been found in many animal and clinical studies to have anti-inflammatory properties, which are beneficial for pain relief. |
Radically reduce your intake of processed foods — Processed foods not only contain chemical additives and excessive amounts of sugar, but also are loaded with damaging omega-6 fats. By eating these foods, especially fried foods, you upset your body’s ratio of omega-3 to omega-6 fatty-acids, which triggers inflammation. Inflammation is a key factor in most pain. |
Eliminate or radically reduce your consumption of grains and sugars — Avoiding grains and sugars, especially fructose, will lower your insulin and leptin levels. Elevated insulin and leptin levels are one of the most profound stimulators of inflammatory prostaglandin production, which contributes to pain. While healthy individuals are advised to keep their daily fructose consumption below 25 grams from all sources, you’ll want to limit your intake to 15 grams per day until your pain is reduced. Eating sugar increases your uric acid levels, which leads to chronic, low-level inflammation. |
Optimize your production of vitamin D — As much as possible, regulate your vitamin D levels by regularly exposing large amounts of your skin to sunshine. If you cannot get sufficient sun exposure, taking an oral vitamin D3 supplement, along with vitamin K2 and magnesium, is highly advisable. Get your blood level tested to be sure you’re within the therapeutic range of 60 to 80 ng/mL year-round. |
Bodywork Methods That Reduce Pain
The following bodywork methods have also demonstrated effectiveness for pain relief and pain management.
• Acupuncture — According to The New York Times,38 an estimated 3 million American adults receive acupuncture annually, most often for the treatment of chronic pain. A study39 published in the Archives of Internal Medicine concluded acupuncture has a definite effect in reducing back and neck pain, chronic headache, osteoarthritis and shoulder pain — more so than standard pain treatment.
• Chiropractic adjustments — While previously used most often to treat back pain, chiropractic treatment addresses many other problems — including asthma, carpal tunnel syndrome, fibromyalgia, headaches, migraines, musculoskeletal pain, neck pain and whiplash.
According to a study40 published in the Annals of Internal Medicine, patients with neck pain who used a chiropractor and/or exercise were more than twice as likely to be pain-free in 12 weeks compared to those who took medication.
• Massage therapy — Massage releases endorphins, which help induce relaxation, relieve pain and reduce levels of stress chemicals such as cortisol and noradrenaline. A systematic review and meta-analysis41 published in the journal Pain Medicine, included 60 high-quality and seven low-quality studies that looked into the use of massage for various types of pain, including bone and muscle, fibromyalgia, headache and spinal-cord pain.
The study revealed massage therapy relieves pain better than getting no treatment at all. When compared to other pain treatments like acupuncture and physical therapy, massage therapy still proved beneficial and had few side effects. In addition to relieving pain, massage therapy also improved anxiety and health-related quality of life.
• Emotional Freedom Techniques (EFT) — EFT continues to be one of the easiest and most effective ways to deal with acute and chronic pain. The technique is simple and can be applied in mere minutes. A study42 published in Energy Psychology examined the levels of pain in a group of 50 people attending a three-day EFT workshop, and found their pain dropped by 43% during the workshop.
Six weeks later, their pain levels were reported to be 42% lower than before the workshop. As a result of applying EFT, participants felt they had an improved sense of control and ability to cope with their chronic pain. In the video below, EFT expert Julie Schiffman, teaches you how to use EFT to address chronic pain.
