
By ANISH KOKA
“The patient in room 1 should be a quick one, its an addon, they just need a prescription for ivermectin”
I’m a bit puzzled by this sentence from my assistant doing his best to help me through a very busy day in the clinic that I’m already behind in. I walk into the room, a script pad stuffed into my hand as I enter the room, to meet a very nice couple. The wife sits patiently with hands crossed on the exam table.
“So, you’re here for Ivermectin?”, I ask.
Why yes, a trip to Texas is planned.. COVID is in the air, the internet, and some important people who have ‘inside knowledge’ have raised doubts about the vaccine. Some other people who quite possibly could be the same people, have also suggested prophylactic ivermectin is the better bet to prevent these good people from catching COVID.
Ivermectin is a drug known to work against parasites. The virus angle relates to in vitro data that suggests Ivermectin inhibits the host importin alpha/beta-1 nuclear transport proteins, which are part of a key intracellular transport process that viruses use to enhance infection by suppressing the host’s antiviral response. In addition, ivermectin may interfere with the attachment of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein to the human cell membrane. Ivermectin demonstrates a broad spectrum of activity in-vitro against a variety of viruses like dengue, Zika, HIV, and yellow fever. Unfortunately, despite this in vitro activity, no clinical trials have reported a clinical benefit for ivermectin in patients with these viruses.
Ivermectin does inhibit Sars-Cov2 viral replication in cell cultures. However, pharmacokinetic studies suggest that achieving the plasma concentrations necessary for the antiviral efficacy detected in vitro would require administration of doses up to 100-fold higher than those approved for use in humans. Even though ivermectin appears to accumulate in the lung tissue, predicted systemic plasma and lung tissue concentrations are much lower than 2 µM, the half-maximal inhibitory concentration (IC50) against SARS-CoV-2 in vitro. Subcutaneous administration of ivermectin 400 µg/kg had no effect on SARS-CoV-2 viral loads in hamsters, though there was a reduction in olfactory deficit and a reduction in the interleukin (IL-6:IL-10) ratio in lung tissues.
Since the pandemic began, there have been a number of small randomized controlled trials of ivermectin in mild COVID patients that show more rapid viral clearance, but not too much else. The prophylaxis data is considerably more sparse, and is of the retrospective variety. Basically take a number of countries that use Ivermectin variably and compare the incidence of COVID in those countries.
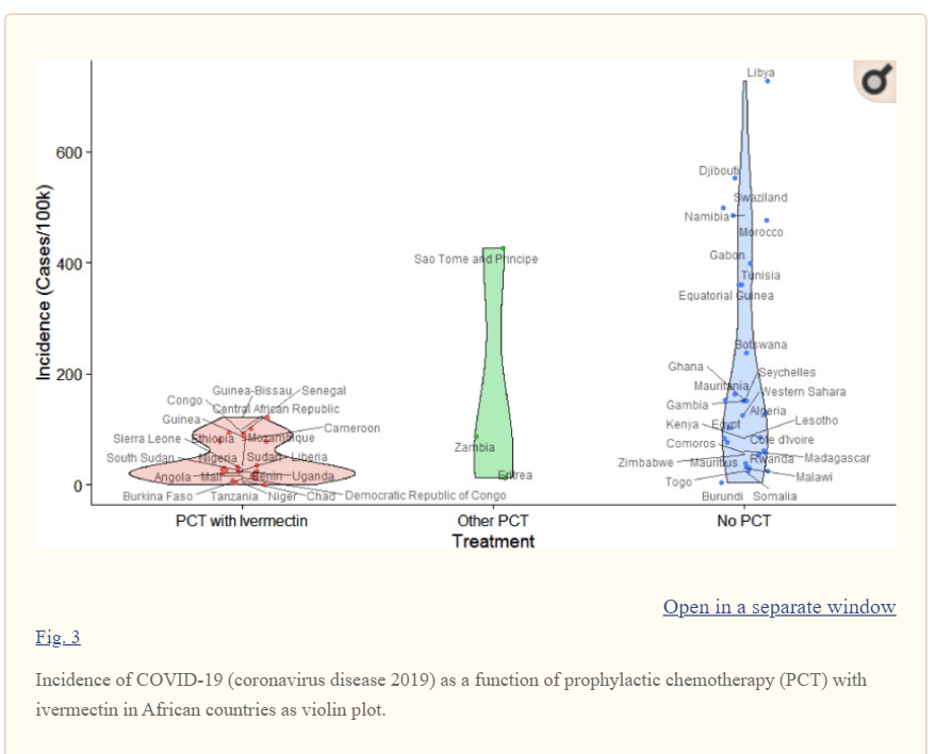
This is the slam dunk data that convinces the nice people in my office, and perhaps a few doctors that Ivermectin, not the vaccine, is what’s best to keep COVID away.
For too many a combination of bioplausibility, personal experience, a 25 person RCT in Lahore, a violin plot pulled from worldometer data from Libya and Sierra Leone, and a distrust of big pharmaceutical companies leads to Ivermectin winning the COVID treatment Game of Thrones.
The problem with large historical (retrospective) datasets is that there is much to fool the casual aggregator of data looking for simple answers. Making sense of data requires understanding of how the numbers arrived at a particular row and column. Mortality may appear to be decreasing in a certain geographical area, but if it doesn’t account for the effects of gentrification pulling from high life expectancy zipcodes, the finding is irrelevant. If it so happens that those leaving have a lower than average life expectancy of the town they’re departing from and higher than the average life expectancy of the town they move to, the average life expectancy of both areas would appear to go up, though no such thing has actually happened! Will Rogers, the famous depression era comedian/actor, son of Cherokee nation and Oklahoma, famous for skewering everyone with good humor, intuited the phenomenon when commenting on the migration from Oklahoma to California triggered by the depression – “When the Okies left Oklahoma and moved to California, they raised the average intelligence level in both states.” It is a fitting tribute to the brilliant comedian who died prematurely in a small plane crash that the concept of grouping data in a way to make both groups appear better is aptly termed the Will Rogers phenomenon.
How exactly one is to organize data is a vexing and not insignificant problem of the retrospective datasets that many use to buttress confident claims because of known and unknown confounders. Confounding occurs when an association between some exposure of interest (Hydroxychloroquine/Ivermectin/Turmeric/Ginger Root) and another outcome of interest (COVID death/incidence) are investigated, but the exposure and outcome are actually associated with a third variable.
A particularly nice explanation with examples is found in a paper in the British Medical Journal that describes situations in which a third variable not only effects the size of the association found, but actually reverses the direction of the effect that was first observed. First described in a technical paper by EF Simpson in 1959, this has come to be known as Simpson’s paradox though the concept has been well understood to many for some time.
Consider an evaluation that took place of diabetics pulled from Poole, a pleasant looking coastal town of south England. The table below is from the excellent book, Dicing with Death by statistician Stephen Senn. It should be obvious a statistician made the table because the term censored is used instead of alive. To a statistician you aren’t alive, you just haven’t died yet which peskily means that the years lived is not yet known, and hence, censored.
The association being studied is insulin dependence and death in the Poole cohort, and in a finding that would surprise everyone, 40% of non-insulin dependent diabetics die, while only 29% of insulin dependent diabetics die.
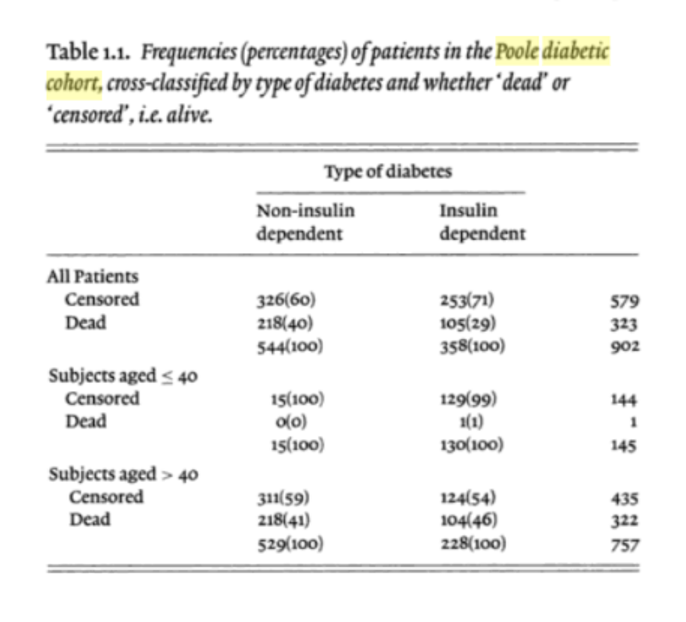
Most involved with the care of diabetics understand what the important third variable here is that needs to be examined : age. Insulin dependent diabetics historically have been much younger, and when the data are examined based on age, the mortality association reverses. A higher proportion of insulin dependent diabetics on both sides of age 40 have a higher proportion of deaths than non-insulin dependent diabetes. The same applies to an analysis of kidney stones that found open surgical treatment was successful 78% (273/350) of the time, while percutaneous nephrolithotomy (1980-5) had a success rate of 83% (289/350), Adding stone size as an important third variable, however finds a percutaneous approach is successful less of often for stones < 2cm, and stones > 2cm. It must be the case then that stone size affects the therapy provided with even more variables not being taken into the analysis like age, frailty, and other medical comorbidities.
The examples provided do involve the arbitrary dichotomization of continuous variables (age 40, stone 2cm), and there are more sophisticated statistical techniques that involve incorporating these factors or covariates to arrive at a smarter answer. This presumes one knows the confounder/factor to look for. Intuiting causation from observational data is a field unto itself and is constantly evolving. There is seemingly always some new method that promises to be the holy grail. I’ll just say that if the holy grail of causation from datasets has been discovered, the pandemic analysis from the loudest epidemiologists on Twitter would appear to be using the holy grail as a urinal. The new purgatory in 2021 is to be stuck between causal inference PhDs obsessed with keeping sixth graders in masks home forever and libertarians overdosing on Vitamin D. (I don’t see any harm in giving Vitamin D to those deficient in Vitamin D!)
A fast moving, novel virus where the large majority of patients would get better if the medical team did a raindance in each patient’s house is exactly the place to be skeptical of retrospective reviews of datasets that find silver bullets, precisely because the potential confounders are surely of infinite number.
I didn’t write for prophylactic Ivermectin because every therapy given has a side-effect profile, the patients in front of me were relatively healthy, and I’m enormously uncertain of the benefit. While doctors like Paul Marik, a famed critical care physician who is the king of spinning therapeutic gold for the very sick from vitamins may be unencumbered by these potential confounders when he claims mortality in his series of vitamin/ivermectin treated COVID patients is 75% lower than the wider world, you should be! COVID is a deadly but incredibly heterogenous disease. There are lots of series of patients with mortality that is very low, even in nursing homes. Find me a disease that we all understand to be morbid from the time of diagnosis — take patients with late stage heart failure requiring inotropes where 6 month mortality is in excess of 75% and show me in that series your favorite vitamin cocktail reduces mortality to 25%.. and I’m all ears. Diseases like COVID where mortality relates to initial dose of virus received, underlying comorbidities, aggressiveness of screening protocols, what the resources of the hospital may be, and what month during the pandemic one goes to the hospital (to name just a few of the known variables) should identify those who have therapeutic certainty in this space as shamans, not messiah’s.
Not all bioplausibility is the same or as easily ascertained. I’ve seen clots transit through holes in the heart, and gone on to write why closing those holes would prevent strokes, but I’ve never seen Sars-COV2 unable to bind to a spike protein in the presence of Ivermectin. The proposed mechanism of action of benefit is speculative, and the clinical effects seen in the trials to date are nothing like when penicillin was used in a petri dish or in humans.
It’s especially galling that this level of evidence has confused members of the public in the face of the available vaccine data. The angst of a brand new mRNA vaccine platform is understandable, but at this point we have tens of thousands of patients months removed from their vaccine enrolled in randomized control trials with next to no significant major adverse events that can be attributed to the vaccine. There were two deaths in the vaccine arm, one from arteriosclerosis, and another from cardiac arrest that may ignite the fires of the QAnon/Russiagate crowd, but these should be quickly doused by the four deaths in the placebo arm (two from unknown causes, one from hemorrhagic stroke, and one from myocardial infarction). None of the deaths were deemed related to either placebo or vaccine.
In striking contrast to the who-knows-effectiveness of recycled anti-parasitic drugs, there’s certainly no beating how incredibly effective the vaccine is. This now famous chart looks at COVID PCR confirmed cases between placebo and vaccine and is very impressive.
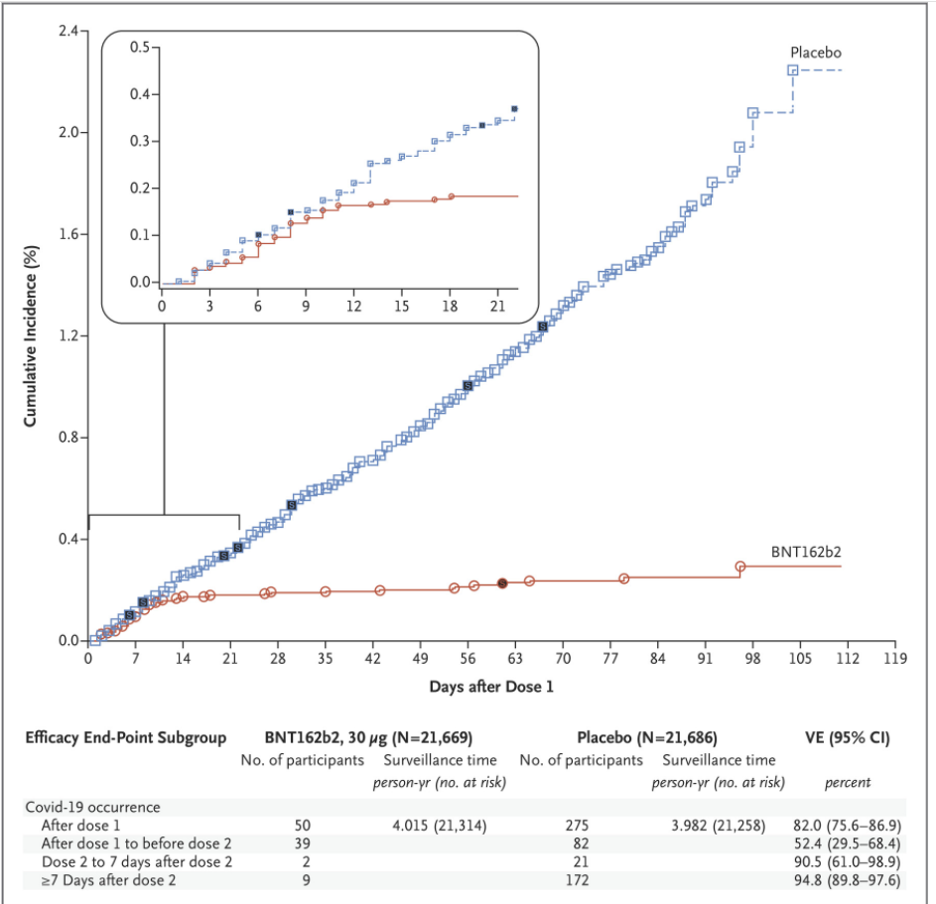
This isn’t taking the continent of Africa and pulling out ivermectin use to relate to COVID incidence, this is randomizing tens of thousands of patients to either vaccine or placebo and observing outcomes Randomization isn’t perfect, but in the COVID space, there’s nothing better.
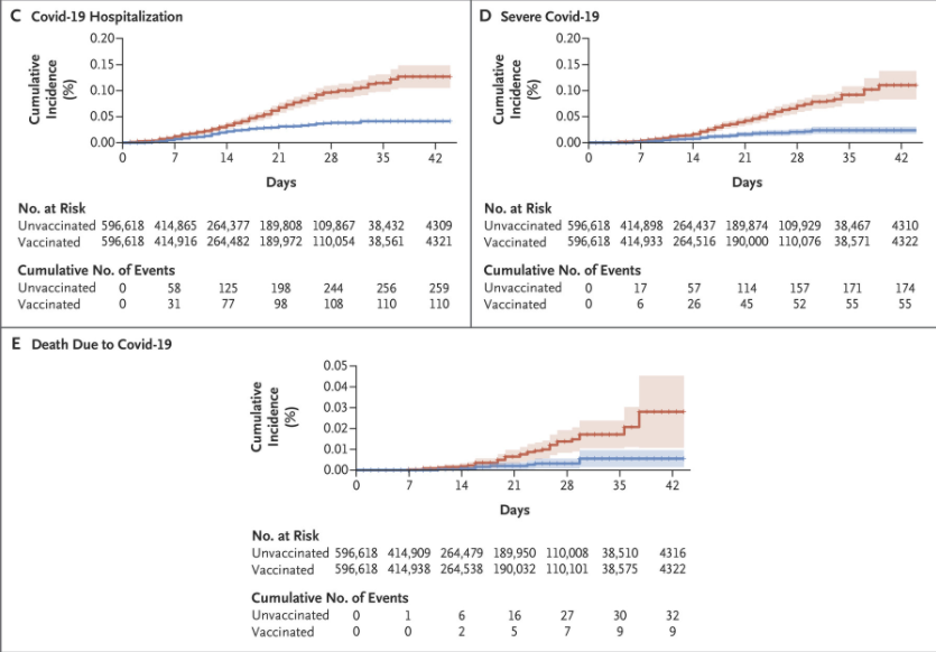
A mild controversy relates to the primary outcome requiring a COVID PCR +ve test. Clearly, there are quite a few patients in the course of the pandemic that clinicians have appropriately labeled COVID +ve despite a COVID -ve test, and adding in all patients reporting symptoms after receiving a shot does significantly attenuate the difference between vaccine and placebo. It’s a reasonable concern, but doesn’t explain the large difference seen in PCR+ve cases, and indeed suggests that many of the symptomatic COVID test -ve patients did not actually have COVID. Regardless, the data that I showed my patients on my phone in the room wasn’t the COVID PCR data, it was the table of severe infections prevented by the vaccine.
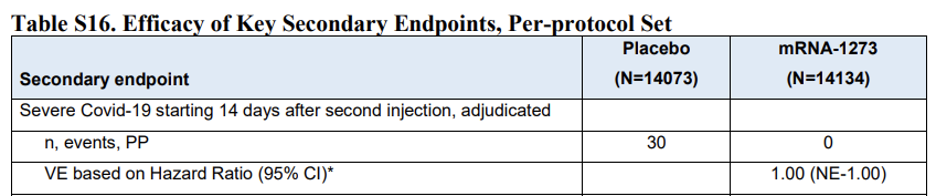
The moderna vaccine data just published earlier this month shows zero, that’s right zero severe COVID infections in the vaccine arm, and thirty in the placebo arm. Analysis of a real world data-set from Israel that compared a matched cohort before and after a mass vaccination program confirms the remarkable findings.
My words to the patients asking for Ivermectin –
“The best way to avoid ending up on a ventilator in the intensive care unit? Take the vaccine!”
The couple left without an ivermectin prescription, but did request to be on our clinic’s vaccine list. I left the room mollified, contemplating how to apologize to the next patient I was now 45 minutes late for.
Anish Koka is a Cardiologist. Follow him on twitter @anish_koka
Spread the love
