While pharmaceutical drugs can sometimes be remarkably helpful, because of how frequently I observe them harm patients, I am inherently hesitant to use them. In each case where they injure someone, I’ve found that typically one or more of the following is at play:
• The drug in question should not be on the market (as it provides significant risk with minimal benefit) but a lot of money has been spent to keep it there because of how profitable it is.
Note: A list of what I currently consider to be the most harmful drugs on the market can be found in this recent article about the acid-reflux industry and this one on the pain management industry.
• The side effects of the drug are conveniently omitted from the literature doctors receive, so when those side effects occur (which suggest the drug should be stopped), doctors frequently don’t recognize them (as you often can’t see something unless you know to look for it) and more importantly they have difficulty believing the adverse reactions could be linked the drug. This is especially true for the more subtle and chronic side effects drugs create.
• The appropriate dose significantly varies from person to person and is often very different from the standard dose.
Every physician I know has specific maxims they follow in their medical practice, and throughout my career I’ve taken many to heart espoused by the most talented physicians I’ve worked with. One of those was:
“I always dose everything.”
In turn, I believe that much of the benefits and harms of each therapy (be it a conventional or holistic one) are the result of the dose that is used. In turn, I frequently observe drugs I do not like (due to their inherent toxicity) greatly benefit patients when they are instead provided at a much lower dose to patients and observe “safe” natural or alternative medical therapies (which I like) harm patients because they were given at too high of a dose.
Low Dose Naltrexone
Your body produces endorphins, which are peptide hormones that activate the opioid receptors in the body and thus function as natural pain killers which create positive feelings for the recipient.
Many of the activities we associate with “feeling good” (e.g., exercise or intercourse) are associated with an endorphin release, and it has been observed that many activities necessary for the survival of our species also are (e.g., breastfeeding causes endorphins to be released and travel into the feeding infant).
Opioid drugs hijack that system and stimulate it at a much higher dose than what the body naturally experiences. This can be both helpful (since that can address severe pain) but also very problematic as the positive experiences opioids create can rapidly become addictive.
That addiction, in turn, is a product of the body recognizing its opioid receptors are being overstimulated by those powerful external opioids and it then creating a compensatory down-regulation of that system to avoid an overstimulation.
Once this happens, the natural endorphin production is no longer sufficient to meet the body’s needs and significant withdrawals occur once opioids are no longer consumed and artificially stimulating that system. There are two important implications of this process.
First it helps to explain why so many drugs (such as those which work on systems besides the opioid receptors) are to varying degrees addictive and why their benefits diminish over time as they are taken chronically.
Conversely, this is why it often works much better to give a drug or supplement intermittently so its signal can clear from the body before a new one is given and in many cases, (such as when treating the cell danger response), pulsed dosing is essential for rebuilding the body’s homeostasis.
Secondly, it raises the question. What if you did the opposite? Because of how addictive drugs can be and how much damage certain addictions create for society, a lot of work has gone into developing protocols for addressing drug addictions.
One approach has been to develop medications (such as naltrexone) which block the body’s opioid receptors, so that when an exogenous opioid (e.g., heroin) is taken, it cannot trigger a pleasurable response, and hence over time causes the addicted individual to gradually lose the desire to consume the opioid.
Note: Naltrexone is often used for other addictions, for example it has been found to be remarkably helpful for alcoholism.
In the 1974, Bernard Bihari MD became New York City’s addiction commissioner (heroin addiction was a huge problem at this time) and ever since was involved in the work being done to combat drug addiction. In 1984, naltrexone was developed, and because of his position, Bihari had followed naltrexone’s development closely, which in turn had caused him to make note of the fact naltrexone had been found to triple the endorphin levels of participants who received it.
A few years before naltrexone hit the market, AIDS had emerged in New York, and since Bihari was seeing many of his addicted patients begin to die from AIDS, in 1985 he switched his focus from addiction to AIDS. Since endorphins were known to regulate the immune response (e.g., injecting them significantly increased immune function in animals) this made him wonder if naltrexone could be used to save the immune-suppressed AIDS patients.
However since naltrexone was difficult for many of his addicted patients to tolerate (as they could not handle the opioid withdrawals it created), Bihari decided to see if a lower dose than 52mg could still achieve a meaningful increase in the body’s endorphins. Before long, he found that 3mg worked as well as 52mg but did not create those significant withdrawals.
He then proceeded to test it on AIDS patients and found that (if administered at the correct time), it dramatically improved the course of the disease. Unfortunately, like many other promising therapies for AIDS, it was given a cold shoulder so Fauci could push the toxic drug AZT onto the market.
Before long, Bihari also discovered low dose naltrexone therapy (LDN) also worked quite well for certain cancers (many cancer treatments essentially work by up-regulating the immune system). Furthermore, he also observed that in both cancer and AIDS, the body’s endorphin levels were about 30% of normal — which may explain why LDN helps so much for those conditions.
Since that time, LDN has also been found to be quite helpful for other conditions, particularly chronic pain and autoimmune disorders (e.g., those caused by the COVID vaccines).
Since a therapy like this threatens numerous pharmaceutical markets, there has always been an institution resistance toward sanctioning the research or use of LDN — however patient advocates have been able to and as time moves forward, more and more evidence of the benefits of LDN have accumulated. In short, LDN illustrates how differently a drug can behave at a different dosage.
How Is a Dose Chosen?
Typically, for a drug to “work,” enough of it has to be present in a patient to trigger the desired effect of the drug. Exactly how much does that varies significantly as:
• The same drug concentrations affect people differently (for example, an opioid user typically requires a higher opioid dose to get high than someone who has never used opioids before).
• Different people require different amounts of a drug in their system to achieve the target concentration of a drug (this is why for example we often give higher dosages to heavier people).
• The degree to which people absorb an oral drug varies significantly (which is one why more toxic drugs are often given intravenously in order to assure a more precise dosing).
• The degree to which people eliminate a drug varies significantly, so in some the drug may clear immediately, while in others it persists for a long time (e.g., some of the drug may still remain when the next dose is taken).
• The content of a drug may vary (especially with off-patent drugs produced overseas).
Note: Many believe this was a major reason why the responses to the COVID-19 vaccines varied so much as the mRNA concentration was found to vary widely in the vaccines tested (along with the presence of contaminants like bacterial plasmids).
Conversely, the toxicity of a drug can widely vary (e.g., for all of the same reasons listed above).
Note: The chronic and more subtle toxicities of a drug receive minimal consideration when dose dependent adverse events are being evaluated.
When drugs are designed, the drug companies thus have to decide what constitutes an appropriate dose for the product. Ideally they want to have minimal side effects while simultaneously having the majority of patients experience the intended effects of a drug. In some cases this is fairly easy, as the toxic dose is much, much higher than the effective dose, while in other cases it’s challenging as the two are very close.
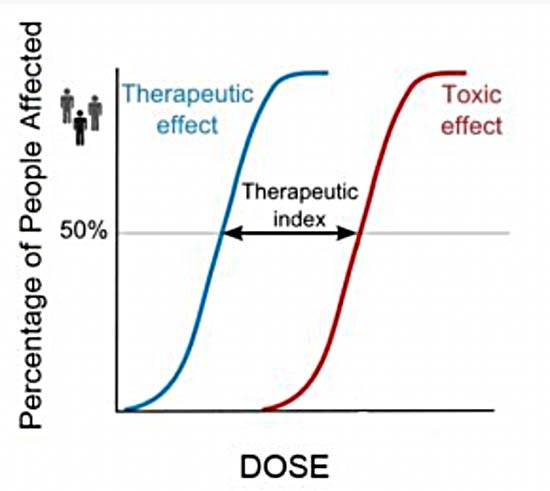
This concept is expressed by the idea of a “therapeutic index,” which quantifies how far the effective dose of a drug is from the toxic dose. With drugs that have a wide therapeutic index, it is relatively unlikely someone taking them as prescribed will experience a known toxicity toxic event, while with drugs that have narrow therapeutic windows, this is much more likely.
For this reason, drugs with narrow therapeutic windows (e.g., chemotherapy — which needs to kill most of the cancer cells without killing too much of the normal cells) are often given in a supervised setting where the exact concentration of the drug can be controlled and side effects can be monitored for.
Note: One of the major problems with the mRNA technology is that since the mRNA doses varied so much lot to lot (as a result of their rushed production), and the time the mRNA persisted in the body also greatly varied, it was not possible to use the existing laws of toxicology to determine what a toxic dose of the COVID vaccines was.
Because it is often impossible to have an effective dose which is low enough that it does not also create side effects in some of the recipients, drug companies typically err towards the higher dose and do their best to downplay the toxicities that occur in their trials. This for example is why in drug trials, the drugs are often only tested on the healthiest members of the population who are the least likely to experience adverse reactions to the medications.
Note: Often when a drug is first launched (especially if it is a new type of medication) the company will use a lower dose of it both in the trials and once it enters the market (as that prevents an initial wave of injuries which may cause the drug to get pulled from the market).
However, once the drug is approved and has become something doctors and patients feel should always be available to them, the dose of the drug and the number of eligible who are eligible to receive it is increased, as at that point, the resulting wave of injuries are unlikely to be recognized or motivate the FDA to upset the public by withdrawing the drug from the marketplace. Later in the article, we will review how this happened with Viagra.
Since the FDA prioritizes signs of efficacy over ensuring safety, as best as I can tell, focusing on “efficacy” has become the industry standard. For example, a key metric the FDA uses to determine if a vaccine should be approved is the antibody response it generates in recipients.
Since different people respond differently to the same vaccination, and there is no penalty for an excessively high antibody response to a vaccine, vaccine manufacturers often create products that overstimulate the immune system.
Prior to the COVID-19 vaccines, one of the best examples of this was the HPV vaccine Gardasil. When it was being designed, Merck realized that it was difficult for the body to develop an immune response to the HPV antigen (which I suspect was due to the body being designed to resist developing autoimmunity and the vaccine’s antigen having similarities to human tissue). To solve this problem, Merck used a much stronger adjuvant.
This “worked” and ensured the vaccine reliably produced an immune response in its clinical trial subjects — but also caused the vaccine to have a very high rate of severe side effects in those who received it. However, since the FDA prioritized “efficacy” this trade off was accepted and ever since then the FDA and CDC have worked hand-in-hand to cover up the immense number of injuries that have been caused by the HPV vaccine.
Note: Many recognized from the start that having a single highly toxic protein (in a rapidly mutating region of the SARS-CoV-2 virus) be mass-produced within the body would lead to a large number of injuries and the virus rapidly mutating to a strain not covered by the vaccine. As such, a longstanding debate has existed over exactly why Pfizer, Moderna (and the FDA which approved their vaccines) chose what was clearly a bad design for the vaccines which would be pushed upon the world.
The least evil explanation I have come up with is that all the vaccine companies knew that whoever was the first to produce a vaccine that appeared to create immunity would get exclusive rights to a massive market.
Pfizer and Moderna in turn prioritized what they thought would be the fastest and most reliable way to do that (using the vaccine to mass produce the most immunogenic part of the virus) in the body, knowing full well that the FDA, in line with its past actions (e.g., towards Gardasil) would ignore the evidence of harm created by this strategy.
Similarly, a case can be made that the reason the experimental mRNA technology was chosen (despite its innumerable safety concerns) was simply that of the existing vaccine platforms, it had by far the shortest production turnaround time.
For context, Fauci and others had worked for years to develop the mRNA platform so that it could be used to make flu shots closer to the flu season, as the existing method required production to start long before it was realistically possible to know what the circulating strains would be (and hence what to put in the vaccine — which is why flu vaccines often have the “wrong” strain each year).
Large Double Blind Trials
At this point in time, we hold the belief that for a clinical trial to be valid, it must have a large number of people enrolled in it, and be double blinded. I would argue the following is true about those trials:
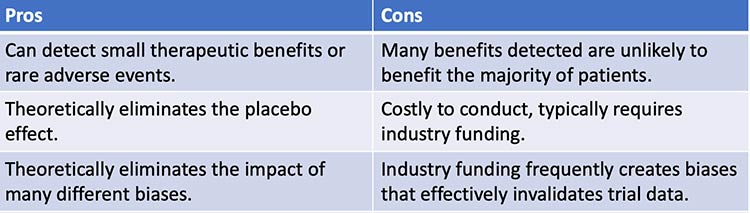
Note: My own belief is that large magnitudes of effect do not require large trials to be detected (which has been repeatedly shown by small studies observing those effects that are eventually confirmed by large blinded trials and then become the standard of care). Since a therapy at least in theory should have a large magnitude of effect, this calls into question the assumed need for prohibitively expense trials in order to adopt a new therapy.
The above also helps to explain why a ton of money is frequently spent on those trials, yet they often fail to detect clinically significant adverse events (e.g., consider the countless severe injuries that whistleblowers from the COVID-19 vaccine trials revealed were covered up by the vaccine manufacturers).
Likewise, financial conflicts of interest help to explain why more and more pharmaceuticals are pushed onto patients despite them not appearing to provide any significant benefit to the majority of those receiving them.
The corruption within the trials is easier to understand (and entirely predictable since their cost virtually guarantees the sponsor will want a positive outcome which protects their investment). However, I believe the fact that they are a weighted average that sees each patient through a collectivist lens rather than as an individual is ultimately much more harmful.
The collectivist lens makes it possible to ensure the overall greatest benefit (e.g., by having the therapy with a 30% success rate rather than the 25% success rate be the standard of care), but it fails to do anything for those who do not benefit from it (which often comprises the majority of patients).
Unfortunately, there is rarely one correct therapy for every patient. For instance, although there are certain things that are more likely to be helpful for COVID vaccine injuries (e.g., improving zeta potential or a systemic regenerative therapy), when working with a vaccine injured patient, I frequently need to use a different approach from what I’ve done before to improve their symptoms).
This reality is fundamentally incompatible with a standardized model which provides the “best” treatment algorithm for every patient.
One of the most important challenges with evidence based medicine hence becomes “how do I know if the results of this trials are applicable to the patient in front of me?” Unfortunately, while some leaders in the field recognize this issue, the majority of physicians in practice do not seriously consider it.
An excellent example is how to dose pharmaceuticals. Many of my colleagues who get the best results with drugs typically use nonstandard doses (normally lower ones) they calibrate to each patient. Because they do this, they are able to get many of the benefits of the drug without much of the side effects.
However, the majority of doctors use the standard dose pharmacies provide the medication in (reflexively assuming it must be correct), thereby failing to recognize that the dose is a weighted average rather than specific to what each person needs. Furthermore, in many cases, those doses are chosen for the sake of making profit rather than serving patients.
For example, as detailed in the memoir of a Pfizer sales rep, when viagra came out, the FDA approved three doses of the medication:
- 25mg — For the elderly (the most likely to use the drug) and those with kidney problems.
- 50mg — The normal starting dose.
- 100mg — For people who did not respond to the starting dose.
Since Viagra was a new medication, Pfizer was worried too many early overdoses (something their trials had detected was a real risk from the drug) would spoil the market.
So, to preempt this, Pfizer broke with the standard industry practice of charging more for a higher dose and made the price for a 50mg tablet and 100mg tablet be the same so that their sales representatives, seeking to meet their monthly quota, would not try to push the higher dose to doctors and cause too many overdoses from the 100mg formulation.
However, this “backfired” as patients quickly realized they could buy the 100mg pill and then cut it in half to save money. Pfizer panicked (as they assumed their initial design made the pill uncuttable) and instructed their reps to instead tell physicians the 100mg dose was optimal. Later, after better solutions were found to prevent patients getting two Viagras for the price of one, Pfizer again reverted to promoting the 50mg dose.
Personalized Medicine
The medical system is structured to follow a “standardized model” which on one hand allows the medical system to effectively distribute complex treatments to the entire population (which in many cases is a phenomenal accomplishment — for example, most of us can get a correctly performed brain surgery if it is needed) but on the other hand falls short for those the standardized model doesn’t work for.
Since our medical system is structured to favor the collective, in order to make it be able to improve and reliably have everyone in it perform as expected, certain biases uphold that paradigm. They include:
Everyone should strive to practice the “best” form of medicine. |
The best form of medicine is that validated by large randomized clinical trials. |
A physician’s personal judgement should be superseded by the existing clinical evidence. |
When conflicting clinical evidence exists, the evidence endorsed by trusted authorities is correct. |
If a patient cannot be helped with the existing approach, rather than the physician trying a new non-standard approach, the patient should be referred to a specialist (who is sadly often a psychiatrist). |
Protecting the medical system is important so if at all possible things that cast doubt on it (e.g., a pharmaceutical injury) should be dismissed. |
As the last few years have shown the world, these biases can create a lot of problem. For example, because the system is so large (and hence has a great deal of inertia) it is very difficult to get anything to become standard of care unless a lot of money is spent to make that happen.
This results in expensive and not necessarily effective therapies (e.g., remdesivir) disproportionately become the standard of care rather than effective low-cost ones no one can profit off of — especially once a lot of money is at stake and corruption inevitably enters the equation.
Likewise, while the standard model creates effective treatments for many conditions (so we no longer have to worry about them), it is poorly suited for recognizing when it falls short and when innovative doctors try to address those short-comings, they are attacked by the medical system. In turn throughout my life, I’ve seen:
- Numerous cases where a bad therapy stayed on the market for years if not decades because everyone who criticized it was silenced and gaslighted (e.g., consider what we just saw with the COVID-19 vaccines).
- Numerous cases where the standard of care failed for patients but effective alternatives met immense hostility from the medical system.
For instance, sepsis is one of the most common causes of death for hospitalized patients, and for this reason, numerous policies and guidelines have been created which aim to improve a septic patient’s likelihood of survival. Nonetheless, hospitalized patients with sepsis still have a 24% – 35% chance of dying and one out of three hospital deaths occurs in a septic patient.
This is noteworthy because if IV vitamin C is given within their first 6 hours at the hospital (along with thiamine and hydrocortisone), the risk of death drops to almost zero. Yet, despite it being repeatedly being shown to do this, most standard doctors won’t consider or administer it regardless of how much patients (or other doctors) plea for it.
Similarly, as we saw throughout COVID-19, the hospital protocols we had to treat it were abysmal, and in many cases were worse than doing nothing — yet there was a steadfast unwillingness to so much as consider any “non-standard” treatment.
This was best illustrated 80 lawsuits (detailed within The War on Ivermectin) where families with a relative being subjected to the COVID hospital protocols, and who was expected to die, had lawyer Ralph Lorigo sue the hospital for ivermectin to be administered to their relative.
Of those 80 lawsuits, in 40 the judge sided with the family, and in 40 with the hospital. Of the 40 cases where ivermectin was given, 38 of the 40 patients survived. Of the 40 cases where the hospitals were allowed to withhold ivermectin, 2 of the 40 patients survived. Yet, rather than taking this as a sign the protocols needed to be reconsidered, the hospitals banded together to create a comprehensive legal strategy that prevented any future lawsuits from succeeding.
In short, I believe that while allowing the best available evidence to dictate the standard of care is a extremely helpful for making a functional medical system, it is not once physicians become so rigidly attached to the viewpoint they are not open to considering “non-standard” approaches when it is clear “standard” ones are failing their patients.
Note: Since there is so much money in medical care now, the system inherently lends itself to corruption, and that corruption has massively increased as the decades have gone by. As a result, much of the “standard of care” doctors are expected to follow exists because someone paid for it, not because it actually helps people.
Why Does Dose Toxicity Vary?
Since I first entered medicine, I observed that some patients were much more sensitive to medications than others were. Yet, each time I tried to raise this point with my supervising doctors, they would insist it had to be something else (e.g., pre-existing psychiatric issues of the patient) because the dose the patient was taking was “appropriate.”
Over time, I began to realize that most people, including doctors, don’t understand how drug doses are chosen and don’t realize that the dose they see is a weighted average that does not account for the more sensitive members of the population.
To a large extent, I sympathize with why things are this way, as it would be very difficult to run a medical system which quickly sees a large volume of patients (e.g., it would take much more than 30 seconds to prescribe the correct dose of a drug), but at the same time, it also makes a large demographics exist for which standard medicine care simply does not work. Some of those demographics include:
• Age — As you become older, your body becomes less able to tolerate toxic pharmaceuticals. For example, the kidneys and liver are responsible for clearing drugs from your body, and since their function declines with age, the elderly often cannot tolerate the same dose of a drug that a younger person can.
Likewise, as you age, your arteries become less able to reflexively bring blood to your head when the blood pressure drops there, and as a result, if we medicate the elderly down to a blood pressure younger adults can easily tolerate, it far too frequently results in them becoming light headed and passing out (which is a huge problem because of the severe harm falls often cause to the elderly).
Conversely, premature infants are less able to tolerate vaccinations than normal weight infants, and as a result, neurological disorders and sudden infant death syndrome following vaccination are much more common in those infants.
Nonetheless, because vaccines are assumed to be a 100% safe and effective, ways to prevent toxic doses (e.g., by vaccinating later in life or spacing out vaccinations) are never considered within the conventional medical system.
• Gender and race — Significant differences exist in how different ages and genders respond to many medications.
Unfortunately, in the same way that drugs frequently given to the elderly are rarely tested on older patients in clinical trials (since to make a drug look “safe” it has to be tested on those least likely to be injured by it — which is typically young healthy adults) it is rare drug trials will assess for gender specific responses to a drug and rarer still that racial differences will be evaluated.
Furthermore, in the name of “diversity, equity and inclusion,” there has recently been a push in the medical field to remove many of the metabolic differences that had been observed between different races (and changed their appropriate medical management).
Note: One reason many suspected SARS-CoV-2 was a race-specific bioweapon is because a lot of research has been done on racial differences in the ACE2 receptor (since many common pharmaceutical drugs target it) and because it was observed that the spike protein’s ACE2 affinity significantly varied by race — something which in theory was possible to design ahead of time due to the preexisting ACE2 research.
• In addition to demographic factors (e.g., age, race, sex) affecting one’s response to a pharmaceutical, genetic variations can as well. For example, the P450 enzymes plays a pivotal role in liver detoxification, and as a result, P450 function directly affects how long a drug will stay in the system and what the resulting appropriate dosage is for it.
On one hand this is periodically considered in medicine since certain drugs (plus a few foods) are known to increase or decrease P450 function (decreasing is more common).
More importantly, significant genetic variations exist in P450 function that are virtually never considered. One of the more tragic examples can be seen with SSRI antidepressants. A long standing problem with those drugs is that a certain portion of people who take them become violently psychotic and then either kill themselves or others (e.g., in a school shooting).
Many of the stories are quite horrifying and subsequent lawsuits those killings initiated showed these side effects were observed throughout the clinical trials and then covered up.
Forensic investigations in turn have been conducted to determine what caused the individuals to turn psychotic. One common thread was the individual having a genetically reduced P450 function, which in turn caused the individual to develop dangerously high levels of the SSRI in their bloodstream.
For example, in one study evaluating 10 patients suspected to have this issue (due to them becoming violent after starting an SSRI), all ten were found to have a genetically altered P450 function, and all ten became normal once their SSRI was terminated.
This is important because very few physicians who prescribe SSRIs are even aware of the P450 issue, so it is something never screened for when the SSRIs are prescribed. Likewise once an individual starts developing early psychotic symptoms, it is rare for the physician to attribute that to the drug (rather they often assume it arises from insufficient dosing and hence give the patient more of the SSRI).
Note: Many other consequential genetic variants have also been identified. William Walsh, PhD for example spent 20 years building a database of 2,800 depressed individuals (which had over 300,000 analyses of blood and urine) and identified five common patterns that were seen.
Most of those patterns in turn were the result of genetic predispositions (e.g., deficient or excessive methylation) that could be detected with relatively affordable tests and if treated directly (e.g., by giving methylation supporting supplements) would resolve the patient’s depression.
In turn, some of these metabolic types would improve if SSRI antidepressants were given to the patient, some would experience no improvement from an SSRI, and some (the over-methylators) would instead begin to turn psychotic if administered SSRIs.
Sadly, while depression is one of the most common reasons why patients see a doctor, very few doctors (including psychiatrists) are even aware of this concept — which again highlights the medcine’s inability to recognize what individuals (rather than the collective) need.
Many other noteworthy examples exist of different responses to pharmaceuticals. For instance, evidence exists showing that some individuals cannot mount a sufficient immune response against the SARS-COV-2 spike protein (as not enough antibodies are produced).
So, if those individuals are vaccinated, they will have free spike protein floating in their blood which then can wreak havoc throughout the body and this was exactly what was found in a study of young athletes who developed myocarditis after the vaccine.
This argues that the vaccine only “worked” for people who would have already been able to survive a COVID-19 infection, which curiously was the exact same thing observed with the early smallpox vaccines — something many (myself included) consider to be one of the deadliest vaccines in history.
Constitutional Archetypes
While the factors I mentioned previously (e.g., age, race, gender, metabolic function and genetic polymorphisms) are sometimes considered when attempting to determine the appropriate dose is for someone, one of the most critical factors is almost never recognized — the individual’s constitutional archetype.
Throughout history, culture’s have observed that certain traits, rather than being evenly mixed throughout the population tend to cluster together in the same people, and in turn, various constitutional archetypes have been identified.
For example, one of the most well-known Western creations is the somatotype theory, which is based off attempting to pair personality traits with specific body shapes which were then classified by linking them to the three germ layers the human embryo develops from.
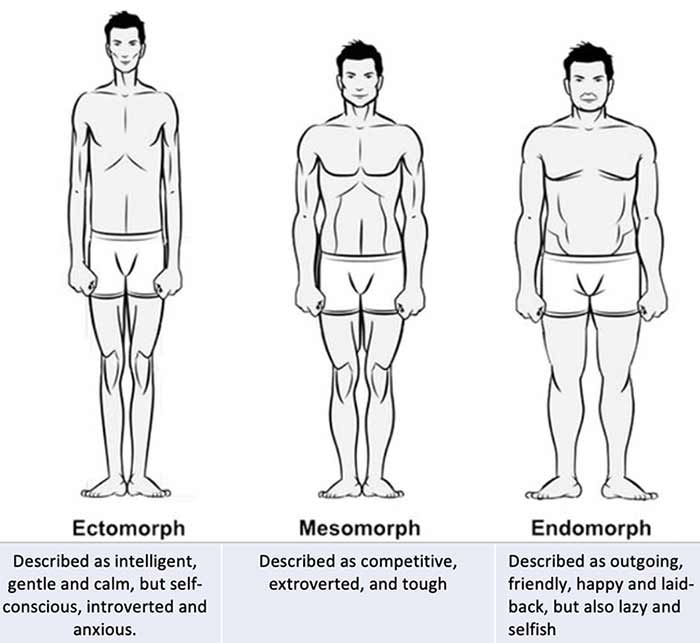
Note: What I find most intriguing about this theory is that I have observed a few instances of individuals having the body type and personality of one somatoform and then later change to the body type and personality of another somatoform.
Of the existing archetypal systems, the one I use the most is Chinese Medicine’s Five Elements, which argues that for anything to physically come into existence, it requires some combination of the five elements to produce that physical manifestation. In turn, each phenomena around us will contain the same combination of the Five Elements that brought it into existence, and hence have a variety of common characteristics reflective of its elemental composition.
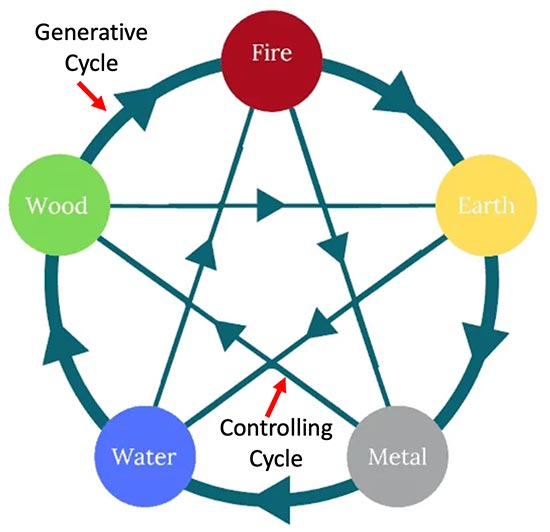
When the Five Elements are applied to medicine, they explain many of the interrelationships within the body, which in turn can frequently be used to predict a susceptibility to illness (e.g., Wood elements are more prone to addiction) and be used to reverse a variety of complex disease processes in the body.
When instead used within a sociological context, they often predict many human behaviors (as each element has certain ways it acts). This is particularly useful in human relationships, as I find much of what determines if people are compatible with each other is a result of the interplay between their elements and if those elements are drawn to each other (e.g., oftentimes people feel drawn to someone else but cannot provide a logical explanation for why it happens).
Note: In the final part of this article, I expand upon the above theme and discuss how one’s Five Elemental constitution influences their behavior in relationships with other human beings (which is often extremely helpful to be aware soon after meeting someone rather than to discover much further down the road).
While the Five Elements are relatively well-known, very few know of the other system I frequently utilize, the Three Gunas from Hinduism — a system which is similar to, but not the same as Ayurveda’s three Doshas.
Guna when translated means something akin to a “quality, peculiarity, attribute, or property.” Three Gunas are recognized to exist, and it is thought in Hinduism that they have always been and continue to be present in all things and beings in the world — although their proportion varies in each place. In turn, the proportion of and interplay between these Gunas defines the character and nature of whatever they imbue. The three Gunas are:
Sattva, which has qualities including “goodness, calmness, harmonious.”
Rajas, which has qualities including “passion, activity, and movement.”
Tamas, which has many qualities including “ignorance, inertia, laziness.”
Sattva in many ways mirrors Vatta, and to a lesser extent the ectomorph type. Rajas in turn pairs with Pitta and mesomorphs while Tamas pairs with Kapha and endomorphs.
The reason I place a heavy emphasis on the three Gunas is because patients will typically have one of the three Gunas predominate them, and the appropriate way to care for them is completely different from someone embodying a different Guna.
Sattvic patients tend to have a more ephemeral (less solid) body type and personality and are much more sensitive to their environment and surroundings. Tamasic patients are the opposite, and tend to have a much denser and thick body type and are much less sensitive to the things around them. Rajasics in turn are the most active of the three and lie in the middle of the spectrum between Sattva and Tamas.
Note: In a recent article, I discussed the curious phenomenon of memories, skills, emotional patterns and preferences transferring from an organ donor to the recipient — something most commonly observed with heart transplants.
One observation made by the researcher who collected numerous highly compelling reports of this occurring was that only a minority of transplant recipients experienced this personality transference, but within that minority, eighteen traits were commonly observed. Interestingly, most of those traits (e.g., an ectomorph body type) were identical to those I typically associate with Sattvic individuals.
This system is important because Sattvic patients tend to be immensely responsive to gentle therapies (e.g., energetic therapies like acupuncture) and react badly to harsh forceful interventions (e.g., having their joints popped, receiving pharmaceuticals or having surgeries). Tamas types are the exact opposite and respond well to forceful interventions while gentle and more natural or energetic ones typically do nothing for them.
There are many consequences of this theory and I would argue the most important one is that it helps guide which type of therapy to use and know ahead of time who will be the most likely to be harmed by it. Throughout my life, I have known Sattvic patients who have been severely injured (and often permanently disabled) by the medical system.
I have always felt this is an immense shame because the sensitivity of the Sattvics often makes them able to perceive what is wrong in the world around them and be driven to fix it, but instead of being able to do any of their critical work they are simply trapped at home by the illness.
In turn, many of the ideas I’ve put forward are strongly influenced by the Sattvics. For example consider the cell danger response (CDR), which I believe is one of the key issues that defines both long-covid and spike protein vaccine injuries (and frequently must be treated to resolve the injury). It was originally developed to answer a simple question — why are some patients (particularly those who eventually seek out integrative medicine practitioners) so sensitive?
For context, these patients have many different hypersensitivities like mast cell degranulation disorder (something also frequently seen following COVID vaccine injuries). Likewise, it is often quite difficult to treat these patients as a tiny amount of a relatively safe therapy would often trigger a systemic decompensation that took them weeks to recover from — something many physicians treating spike protein injured have likewise encountered.
Note: There has also been a longstanding observation within the integrative medical field that hypermobile patients (e.g., those with Ehlers-Danlos syndrome) are much more “sensitive” and likely to be injured by pharmaceuticals (e.g., the HPV vaccine). I have noticed those patients tend to have a Sattvic constitution.
I find that outside of the integrative field, Sattvics are relatively misunderstood by the medical field, and as a result, their sensitivities are often interpreted to be psychiatric in nature. Further compounding the issue, since there are also many Tamasic patients (who respond quite well to conventional care), mainstream doctors tend to disproportionately remember those positive responses and assume they generalize to their entire patient population.
So when the opposite of what the physician intends ultimately happens from their treatment plan, they tend to view it as being fault of the patient rather than consider that they might be working with a different constitutional archetype which intrinsically requires a different treatment approach or at the very least a different dose.
Likewise, I tend to notice that healers (both doctors and non-doctors) tend to gradually accumulate a practice matching the Guna the physician is unconsciously biased towards treating.
Selecting the Correct Dose
All of this article hence begs the question — how does one determine what the correct dose is for a patient? I believe the single most important thing is simply the awareness the dose you assume you should use may or may not be correct. In turn I typically use a few strategies:
Do what I can to become aware of the therapeutic window of the medication I am using. Some medications are fairly safe and extremely unlikely to create issues at normal doses in most patients, others are much more likely to cause issues for some of the people you give them to. The primary problem with this strategy is that it requires you to be honest with yourself over the side effects the medications you prescribe cause and I frequently observe well-intentioned doctors being able to spot if drugs other doctors prescribe cause issues but almost never are able to see when theirs do the same thing. Note: Even though I am a fan of LDN (and it is often very helpful for things like COVID-19 vaccine injuries), I’ve also seen a quite a few people who do not respond well to it or test for it. Similarly, I’ve seen numerous patients who looked like a perfect fit for LDN, but once they started it got worse and eventually learned that if someone is too depleted, they cannot tolerate the small endorphin blockade LDN initially creates. This in turn has gotten me into numerous arguments with integrative colleagues I shared patients with since LDN (understandably) has earned such a good reputation in the integrative medical field. |
Have labs you are familiar with that can determine if a patient is at a higher risk from a specific pharmaceutical and indicate if the desired effect of a medical regimen are occurring or if any unwanted effects are occurring. I am personally not a fan of this approach because it is often quite costly for the patient, and I feel the lab results (especially the newer non-standard ones) often have a very weak correlation with how the patient is doing (which many are now discovering for COVID vaccine injured patients). However, while I and most of my colleagues are not as lab focused in our practice, I also know holistic physicians who have taken the time to really understand a few of them and effectively use them to guide appropriate dosing for their patients. |
Be aware of what nutrients drugs commonly deplete in the body, and be able to recognize if your patient may have a pre-existing deficiency of that nutrient prior to when you start the pharmaceutical. Note: Suzy Cohen, in her book Drug Muggers has made a good case that many of the side effects we attribute to medications are a result of them causing critical nutritional deficiencies. |
Evaluate if I am dealing with a more sensitive or Sattvic patient and adjust my dosing accordingly (which is frequently less than 10% of the normal dose). |
Learn what can be expected to occur with lower doses of a pharmaceutical. |
Start with a lower than normal dose of a therapy, evaluate what happens, and if it seems justified (no harms have occurred and the benefits are not sufficient for the patient), gradually raise it. This approach is much less likely to create adverse events for a patient, but it also much more time consuming to do, so patients who have not already been injured by pharmaceuticals are often unwilling to tolerate continuing to experience their symptoms as they wait for you to gradually increase them to an appropriate dose. For this reason, it’s important to have patients who are willing to go slowly and can afford the extended number of visits doing this requires. In many cases this is simply not viable, and both I and many of my colleagues have had numerous cases where we escalated a dose for a desperate patient faster than we had originally planned to and then regretted doing so once they had a significant reaction to that (still relatively low) dose. Note: Evaluating the effects of the therapy requires frequently carefully observing the patient for subtle signs of a change — as subtle signs the body is not tolerating a medication typically emerge before more overt ones. |
As a result, figuring out how to balance all of these constraints is a bit of an art. Fortunately there are a few unorthodox tricks people have found over the years that greatly help.
Note: Appropriate dosing does not only apply to pharmaceuticals — it can apply to everything you suggest to patients. For example, I’ve found red-light therapy (like the ones discussed here) can be extremely helpful for vaccine injuries, but only if they are dosed appropriately and I recently had a patient share that they had a profound improvement in their quality of life once they had learned how to correctly self-dose the red-light therapy I had prescribed to them.
Lastly, the ideas laid out here also should be considered by patients. If you experience an adverse change or something simply feels wrong, you should be open to the possibility it is due to the drug (or the new dose of a drug).
Many patients who developed chronic injuries from a toxic pharmaceutical have told me that one of their greatest regrets was listening to their doctor instead of their intuition or their body when they decided to go forward with taking the pharmaceutical that then ruined their life.
The Art of Medicine
One of greatest challenges faced by science is to create a model of nature’s complexity which is accurate enough to meet the needs of society. For instance, since the body is so complicated, the simplified treatment models medicine creates (e.g., what dose to use) often fall short.
Medicine is often referred to as both an “art” and a “science.” In my eyes, the “art” of medicine is a recognition of the fact so much is occurring within the human body mind and spirit that knowing what is correct to focus upon can only be identified by the artistic capacity of the human soul.
In turn, all of the most successful medical practitioners I know (e.g., those who are able to solve cases dozens of other doctors could not), like artists in many other fields integrate three different skillsets together:
- A high degree of knowledge and critical thinking with the subject at hand.
- A high degree of proficiency in the task they are attempting to accomplish.
- A highly refined intuitive capacity which provides them insights into where to focus their attention with each patient and discern which concepts are most applicable for each patient.
Note: The traits of the physicians who could do all three of these (e.g., they tend to be the lone dissenters from dysfunctional narratives like the COVID vaccines) is discussed here.
Early on, I realized the importance of all three, as over and over again, I saw patient situations that were simply too complex to figure out without some type of intuitive framework to guide your clinical decision making.
Conversely, I came across more cases than I can count of individuals who relied upon their intuition, but were mostly unable to help their patients as critical gaps existed in their basic knowledge or skillset that were needed for the case at hand (and likewise made them unable to make sense of what their clinical intuition detected).
Unfortunately, since much of our culture has disconnected the mind and spirit from the physical body, it is often taboo to discuss how things like intuition pertains to the practice of medicine.
For instance one of the most well-known methods utilized within integrative medicine to determine the correct dose of a medical therapy (or even what therapy to use in the first place) is “applied kinesiology” or “muscle testing.”
Yet despite the fact this approach is well-known and widely practiced, many who use it (including numerous prominent figures in the integrative medical field I’ve spoken to) won’t publicly admit to doing as such — which in my eyes against illustrates just how taboo it is to discuss the less physical aspects of medicine.
Note: “Muscle testing” is understandably a very controversial topic. I’ve spent years trying to figure out why it works and what can be done to make it more consistent (as there is significant variability when less skilled practitioners utilize it). My perspectives on that subject and the ways to best make use of muscle testing can be found at the end of this recent article.
A Note From Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician in the Midwest and a longtime reader of Mercola.com. I appreciate his exceptional insight on a wide range of topics and I’m grateful to share them. I also respect his desire to remain anonymous as he is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
